After completion of this session the participant should be able to:
Lack of oxygen supply to organs before, during or immediately after birth results in asphyxia which is recognized by either delayed onset of breathing/ cry with/ without need for assisted ventilation.
Clinical features that these babies evolve over the first 2-3 days of life include irritability or coma, hypotonia or hypertonia, convulsions, apnea, poor suck and feeding difficulty. The diagnosis in preterm infants is difficult, as they may be hypotonic because of prematurity.

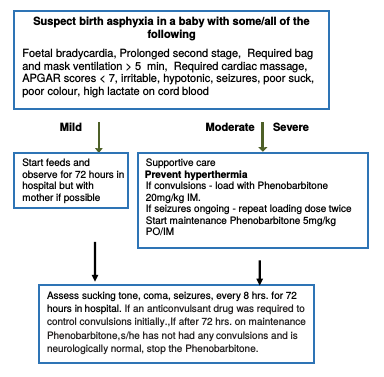
Classify the degree of Hypoxic Ischaemic Encephalopathy (HIE) according to the table below. Babies with mild and moderate HIE generally have a good prognosis and generally do well. An infant who, within a week of birth, is still floppy or spastic, unresponsive and cannot suck has a severe brain injury and will do poorly.
| FEATURE | Mild | Moderate | Severe |
|---|---|---|---|
| Consciousness | Irritability | Lethargy | Comatose |
| Tone | Hypotonia | Marked hypotonia | Severe hypotonia |
| Seizures | No | Yes | Prolonged |
| Sucking/ respiration | Poor suck | Unable to suck | Unable to sustain spontaneous respiration |
| Key facts for provider’s - supportive management of birth asphyxia
Check for emergency signs ABC and provide emergency care Place these babies under radiant warmer to maintain normal temperature but prevent hyperthermia Check blood glucose and if hypoglycaemia is detected. Treat. If not hypoglycaemic check blood glucose every 12 hrs. Fluids: In a baby with emergency signs (breathing difficulty, shock, coma or convulsions), provide maintenance intravenous fluids and according to age after initial stabilisation of emergency signs. Feeding: If the baby has neither emergency signs nor abdominal distension, consider enteral feeding. If the baby is sucking well, initiate breastfeeding or initiate tube feeding with breast milk in those with poor/no sucking using wall charts to determine the volume. |
| Convulsions | Jitteriness |
|---|---|
| Have both fast and slow components Slow movements (1-3 jerks per second) | Fast movements (4-6 per second); tremors are of equal amplitude |
| Not provoked by stimulation | Provoked by stimulation |
| Does not stop with restraint | Stops with restraint |
| Neurological examination-often abnormal | Neurological examination-usually normal |
| Often associated with eye movements (tonic deviation) | Not associated with eye movements or autonomic changes |
For manangement of coma and convulsions see:
Document in health passport and classify HIE as mild, moderate or severe.
If severe arrange follow up at six months - focus on head growth, general health and motor neurodevelopment. Assessments at 12 to 24 months focus on cognitive skills and language development.